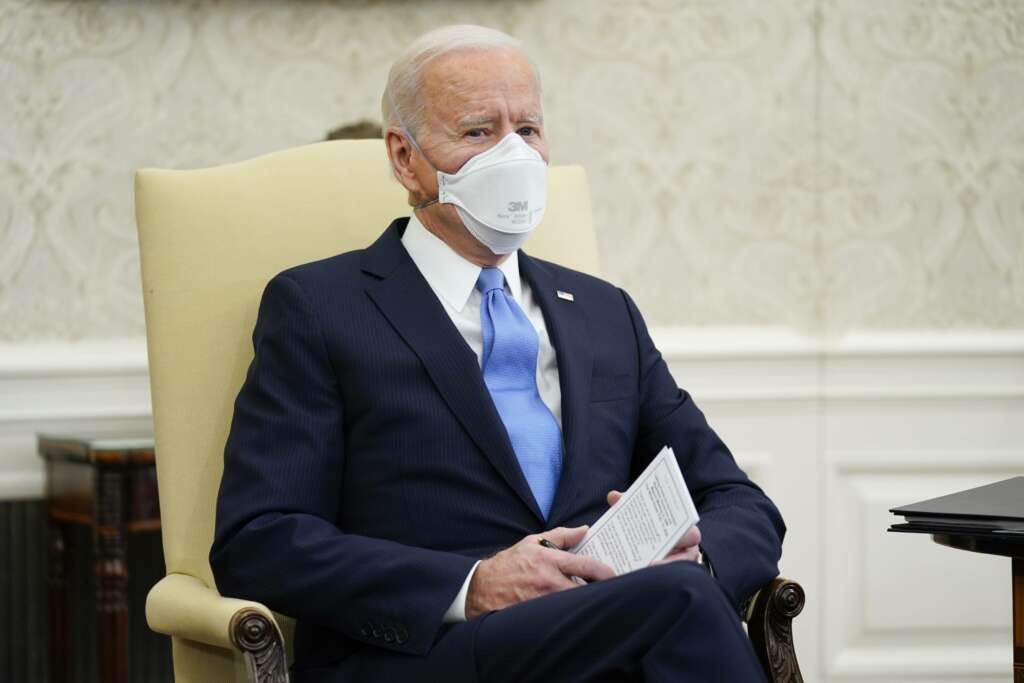
WASHINGTON (AP) — The Biden administration is moving to roll back Medicaid work requirements in its latest effort to undo a controversial Trump-era policy.
Federal health officials planned Friday to inform 10 states that they would revoke permissions granted by the Trump administration to impose such requirements, according to a Biden official who spoke on condition of anonymity to discuss internal plans. Officials were also set to withdraw the past administration’s invitation for states to apply for approval for work requirements.
The move, which was first reported by the Wall Street Journal, follows an executive order Biden signed last month that directed officials to review and remove barriers to Medicaid coverage.
Medicaid is a $600 billion federal-state program that covers about 70 million people, from pregnant women and newborns to disabled people and elderly nursing home residents. Under the Obama-era Affordable Care Act, states gained the option of expanding the program to many low-income adults previously ineligible. More than 12 million people have gained coverage as a result.
The Trump administration allowed states to require “able-bodied” adults drawing Medicaid benefits to work, volunteer or study.
Before the pandemic, nearly 20 states had tried to implement requirements after the administration invited them in 2018 to submit such proposals. A federal judge blocked the requirements in Arkansas and New Hampshire, as well as in Kentucky, before the state’s Democratic governor reversed course and dropped its requirements. Two other states, Arizona and Indiana, have blocked enforcement or implementation, citing litigation.
Arkansas Attorney General Leslie Rutledge called the decision by the Biden administration an “overreach of executive power.”
“It is unfortunate that President Biden and his administration felt compelled to take steps to withdraw the approval of Arkansas’s work-requirement pilot program without giving it an opportunity to succeed,” she said in a statement. “The one-size-fits-all Medicaid program doesn’t work.”
Arkansas was the first state to implement the program, but a 2020 study conducted by Harvard University health researchers found that in the 10 months before the program was put on hold by a judge, 18,000 Arkansans lost coverage, and the program did not increase employment.
A statement from the Centers for Medicare and Medicaid Services highlighted the coronavirus pandemic — with high unemployment exacerbating the public health crisis — as a key concern in ensuring Americans face no roadblocks to getting health care.
“In the midst of the greatest public health emergency in generations, now more than ever, people with Medicaid need access to care,” the statement reads. “This is not the time to experiment or test policies that risk a substantial loss of health coverage or benefits, especially for individuals and communities significantly impacted by COVID-19 and other health inequities.”
Copyright © 2021 . All rights reserved. This website is not intended for users located within the European Economic Area.